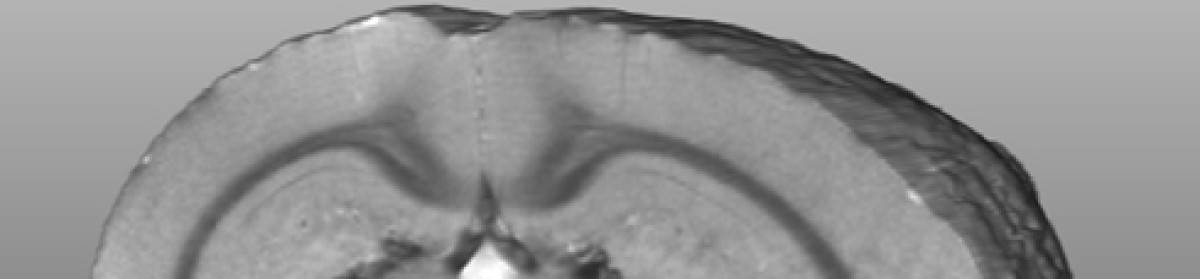
Diffusion tensor MRI showing breaks on long fibre tracts when myelin is lost. This example is from a model of multiple sclerosis. See explanation below. Thanks to the team at the Experimental Imaging Centre and Dayae Jeong.
Diffusion tensor MRI showing breaks on long fibre tracts when myelin is lost. This example is from a model of multiple sclerosis. See explanation below. Thanks to the team at the Experimental Imaging Centre and Dayae Jeong.
What is injured in your brain after a concussion? It is pretty obvious that something isn’t quite right. There is a list of symptoms in the sport concussion assessment tool three, the SCAT3, that you can look at for a range of symptoms.
http://bjsm.bmj.com/content/47/5/259.full.pdf
The brain has long communicating fibre bundles called nerve tracts. These are clearly visible on MRI. The problem that MRI researchers have had in the past is that the changes are very subtle and not visible on standard MRI’s.
To overcome this problem, MRI groups have been working intensely to make the images more sensitive to the injury. There are MRI methods, called “sequences” by MRI specialists, which are showing promise as being sensitive to structural injury. These sequences are sensitive to the amount of myelin. Myelin is the covering on nerves that helps the signal travel down the nerve. When you lose myelin, as occurs in conditions such as multiple sclerosis, the nerve doesn’t function as well. If the myelin doesn’t regrow, the nerve may die.
Clinical MRI systems are actually imaging protons and the most abundant source of protons in the body is in water. So MRI is really imaging water. The trick to making contrast in the image is to make the sequence sensitive to things that can change in the water.
For instance, water can diffuse or move. In the brain, water diffuses fairly readily along fibre tracts but does not readily diffuse across a tract. This is because myelin is similar to soap, and it repels water. An MRI sequence called diffusion tensor imaging has emerged which is sensitive to the amount of water and the direction the water is diffusing. If water diffuses randomly in all directions, it is called anisotropic diffusion. If the diffusion has a directionality, it is isotropic. The measure of this is the fractional anisotropy or FA.
If myelin is damaged, water can more readily diffuse in all directions and the FA will decline. Such changes have been observed indicating that myelin may be damaged in certain regions of the brain after mTBI.
Dean, P. J., J. R. Sato, G. Vieira, A. McNamara and A. Sterr Long-term structural changes after mTBI and their relation to post-concussion symptoms. Brain Inj: 1-8.
Shenton, M. E., H. M. Hamoda, J. S. Schneiderman, S. Bouix, O. Pasternak, Y. Rathi, M. A. Vu, M. P. Purohit, K. Helmer, I. Koerte, A. P. Lin, C. F. Westin, R. Kikinis, M. Kubicki, R. A. Stern and R. Zafonte A review of magnetic resonance imaging and diffusion tensor imaging findings in mild traumatic brain injury. Brain Imaging Behav 6(2): 137-92.
Another sequence that looks at myelin is called quantitative T2. A very specific, not widely available variant is called imaging myelin water fraction or MWF. The University of British Columbia MRI group has been a leader in this area. They looked at MWF in athletes and, indeed, found reduced MWF along major fibre tracts in brain. http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0150215
Again, this supports the idea that damage to myelin occurred.
Wright, A. D., M. Jarrett, I. Vavasour, E. Shahinfard, S. Kolind, P. van Donkelaar, J. Taunton, D. Li and A. Rauscher (2016) Myelin Water Fraction Is Transiently Reduced after a Single Mild Traumatic Brain Injury – A Prospective Cohort Study in Collegiate Hockey Players. PLoS One 11(2): e0150215.
Another sequence is called magnetization transfer imaging or MTI. This one looks at how water interacts with surrounding chemicals and how those chemical transfer some of their MRI related characteristics (or magnetization) to water. This is where the label “magnetization transfer” arose. One can design a sequence such that a lot of magnetization is transferred to water if myelin is present, but not much if myelin is not present. So the MT declines as myelin is lost.
There has been less work on MTI, but I expect to see a lot more. What has been done though, is consistent with the other methods. A decline in MT has been observed.
McGowan, J. C., J. H. Yang, R. C. Plotkin, R. I. Grossman, E. M. Umile, K. M. Cecil and L. J. Bagley (2000) Magnetization transfer imaging in the detection of injury associated with mild head trauma. AJNR Am J Neuroradiol 21(5): 875-80.
Narayana, P. A., X. Yu, K. M. Hasan, E. A. Wilde, H. S. Levin, J. V. Hunter, E. R. Miller, V. K. Patel, C. S. Robertson and J. J. McCarthy (2014) Multi-modal MRI of mild traumatic brain injury. Neuroimage Clin 7: 87-97.
So, there are three MRI methods that have been used to show a loss of myelin after concussion or mTBI. This is worrying as it is very difficult to re-grow myelin to its original form. It is encouraging as there are imaging methods on the horizon that may help identify the extent of injury after concussion.
Diagnosing concussion is one thing, and we probably do that pretty well now. However to manage the injury we need to know the magnitude of the injury, where the injury has occurred, and whether the injury has recovered. This is the holy grail of brain imaging in the field of concussion research.